The 2016 Great Strides Walk in Jacksonville is over and we are so glad we went. The Jacksonville walk is probably the smallest walk we've been a part of, but it was really enjoyable.
Great Strides was held at the University of North Florida campus and let me tell you, it's just beautiful. Definitely makes me want to retire and go back to school! I'll probably never do it, but I'd like to do it anyway.
Team Sam was joined this year by two of my shipmates from the USS Hue City. BM3 Melynn Cobaugh and FC2 Jonathan McDonald, joined by their significant others, brought their experiences with CF to our team. My sincere hope is that we are forming the bonds of teamwork that will be amazing next year. Our ship won't be in Jacksonville for next year's walk, so we'll have to get creative, but we've done some cool things before.
Here's the 2016 Team Sam pictures!
Sam had already run ahead of us on these next few pictures, but we found her sign!
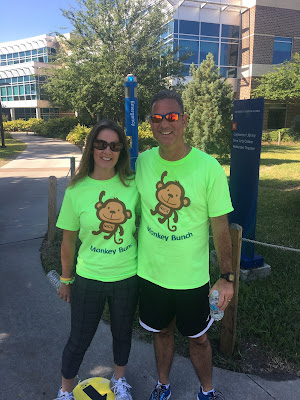
We always love seeing some of the cool t-shirts that teams wear. Here are a few I liked in particular:
We could always use your financial support for our Cystic Fibrosis Team. Please consider donating by clicking this link.
Here's to 2017!
Great Strides was held at the University of North Florida campus and let me tell you, it's just beautiful. Definitely makes me want to retire and go back to school! I'll probably never do it, but I'd like to do it anyway.
Team Sam was joined this year by two of my shipmates from the USS Hue City. BM3 Melynn Cobaugh and FC2 Jonathan McDonald, joined by their significant others, brought their experiences with CF to our team. My sincere hope is that we are forming the bonds of teamwork that will be amazing next year. Our ship won't be in Jacksonville for next year's walk, so we'll have to get creative, but we've done some cool things before.
Here's the 2016 Team Sam pictures!
I took a few selfie pics of the entire team. As you can tell, I had no real idea what I was doing.
Sam had already run ahead of us on these next few pictures, but we found her sign!
We always love seeing some of the cool t-shirts that teams wear. Here are a few I liked in particular:
We could always use your financial support for our Cystic Fibrosis Team. Please consider donating by clicking this link.
Here's to 2017!